Supplementation of the population during the COVID-19 pandemic with vitamins and micronutrients - how much evidence is needed?
Swiss Med Wkly. .. 2021 May 19;151:w20522. doi: 10.4414/smw.2021.20522. eCollection
Philipp Schuetz 1 Philipp.Schuetz at unibas.ch, Claudia Gregoriano 2, Ulrich Keller 3
Download the PDF from VitaminDWiki
Table of contents
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2) has led to a global pandemic with severe respiratory disease and high morbidity and mortality [1]. In turn, there has been an unprecedented research effort to improve the understanding of pathophysiological mechanisms, risk factors, diagnostic tests, and measures for effective prevention and treatment of COVID-19. Age and age-related vulnerabilities - such as malnutrition and frailty - have emerged as the major risk factors for adverse clinical outcome and mortality in patients with COVID-19 [2]. Higher age is a general risk factor in most illnesses, but it is possible that the high fatality rate among the elderly frail population may be explained - at least in part - by deficiencies in specific vitamins and micronutrients, which are vital for a well-functioning immune system.
Over the last decades, many preclinical and observational studies have provided evidence that vitamins and micronutrients play an important role in the efficient functioning of the immune system. As a consequence, deficiencies in these vitamins and micronutrients may reduce the immune response of patients and increase their vulnerability to infections and to have more severe courses once infected. Vitamin C, for example, is an essential vitamin that cannot be synthesised by humans as a result of loss of a key enzyme in the biosynthetic pathway [3]. Severe vitamin C deficiency results in scurvy, which is characterised by weakening of collagenous structures, poor wound healing and impaired immunity with high susceptibility to fatal infections such as pneumonia [4]. Similarly, vitamin D has been shown to influence susceptibility to and severity of infection via multiple mechanisms with a direct impact on production of the antimicrobial peptide cathelicidin and different cytokines via the innate and adaptive immune system, as well as via the NFkB (nuclear factor kappa-light-chain- enhancer of activated B-cells) pathways [5].
One straight-forward “public health” approach would be to start vitamin and micronutrient supplementation of the entire population at risk to reduce the risk for deficiencies and thereby reduce vulnerabilities. Such an approach may be most suitable for interventions with high clinical efficacy, a high proportion of the population showing benefit, proof of safety and overall low treatment costs. Recently, several researchers from Switzerland have published a call for action to consider supplementation of high-risk groups with micronutrients and vitamins as a strategy to diminish adverse health consequences of COVID-19 in the Swiss population [6]. Clearly, supplements and vitamins are over-the-counter medications with excellent safety data and relatively low treatment costs. Still, to be a valuable public health strategy, evidence of clinical efficacy of broad vitamin and micronutrient supplementation of the population in question is needed. Whether this is the case for vitamins and micronutrients in the face of the COVID-19 pandemic needs further exploration and will be discussed in this brief review.
Deficiencies of specific micronutrients and risk of infections
There is evidence from preclinical and observational clinical studies that specific vitamins and micronutrients play a major role in immunity, and that deficiencies are related to higher risks for infection and adverse clinical outcomes [6]. Indeed, there is wide consensus about the importance of several vitamins (vitamins A, B6, B9, B12, C, D and E), trace elements (zinc, iron, selenium and copper) and omega-3 long-chain polyunsaturated fatty acids (n-3 PU- FA) for a well-functioning immune system [7]. As yet, these relationships are best documented for vitamin D and vitamin C [3-5]. Because deficiencies in vitamins and micronutrients are rarely isolated, but mostly in conjunction with general malnutrition and thus deficiencies in multiple nutrients, interpretation of studies regarding single compounds is challenging.
Vitamin D deficiencies in Switzerland
In Switzerland, there is a high number of patients with vitamin and micronutrient deficiencies, particularly among the elderly population. It has been estimated by the Swiss Federal Office of Public Health that large parts of the Swiss population have inadequate serum 25-hydroxy-vitamin D (25(OH)D) concentrations, particularly among the elderly, frail population. For example, a recent clinical multicentre study found that 60% of multimorbid medical inpatients had deficient vitamin D levels (<50 nmol/l) on admission and 25% were severely deficient (<25 nmol/l) [8]. In this study, vitamin D deficiency was associated with a 30% increase in mortality risk in a statistical regression model adjusted for demographics and comorbidities. Similar to other observational studies, however, the study could not allow causal inference and thus provide proof that supplementation with vitamin D would be effective in reducing excess mortality in patients with deficient levels. Several other studies have also confirmed that the vitamin D status of the Swiss population is inadequate for vulnerable populations groups (e.g., pregnant women, older adults, multi- morbid patients), particularly during the winter season. For other vitamins and micronutrients, intake and levels in the general population have not been studied extensively recently.
Evidence from observational trials
In light of their important role regarding immune function, deficient levels of specific vitamins and micronutrients may increase the risk of acquiring an infection and of adverse outcome among infected patients. Most research looking at associations of vitamin and micronutrient deficiencies and clinical outcome was done in the years before COVID-19; however, today there are also several studies investigating levels of vitamins, mainly vitamins D and C, in COVID-19 patients. Table 1 provides an overview of currently published observational studies (upper part of the table) on the association of vitamin and micronutrient deficiencies and clinical outcomes in the population of patients with COVID-19. These studies, from several countries, suggest that for COVID-19 such associations are also present, particularly for vitamins D and C, although there is some heterogeneity among studies and some studies have not reported significant findings. This heterogeneity may be due to various reasons including differences in patient populations, differences in analytical methods, low number of patients in some studies (resulting in low power) and differences in outcomes assessed. As an important limitation of all observational research, levels of vitamins and micronutrients are strongly correlated with age, malnutrition and burden of chronic illnesses, and confounding is a major issue in this type of observational research.
Vitamin D Clinical Trials
A small subset of the data, sorted - tables in PDF include other nutrients
- NCT03188796 The VITDALIZE Study: Effect of High- dose Vitamin D3 on 28-day Mortality in Adult Critically III Patients Austria, Belgium
- NCT04334005 Vitamin D on Prevention and Treatment of COVID-19 Spain
- NCT04344041 COvid-19 and Vitamin D Supplementation: a Multicenter Randomized Controlled Trial of High Dose Versus Standard Dose Vitamin D3 in High-risk COVID-19 Patients (CoVitTrial) France
- NCT04363840 The LEAD COVID-19 Trial: Low-risk, Early Aspirin and Vitamin D to Reduce COVID-19 Hospitalizations
- NCT04370808 VITACOV: Vitamin D Polymorphisms and Severity of COVID-19 Infection Portugal
- NCT04385940 Vitamin D and COVID-19 Management
- NCT04386044 Investigating the Role of Vitamin D in the Morbidity of COVID-19 Patients UK
- NCT04386850 Oral 25-hydroxyvitamin D3 and COVID-19 Iran
- NCT04394390 Do Vitamin D Levels Really Correlated With Disease Severity in COVID-19 Patients? Turkey
- NCT04403932 Increased Risk of Severe Coronavirus Disease 2019 in Patients With Vitamin D Deficiency Spain
- NCT04407286 Vitamin D Testing and Treatment for COVID 19 USA
- NCT04411446 Cholecalciferol to Improve the Outcomes of COVID-19 Patients Argentina
- NCT04435119 Covid-19 and Vitamin D in Nursing- home France
- NCT04449718 Vitamin D Supplementation in Patients With COVID-19 Brazil
- NCT04459247 Short Term, High Dose Vitamin D Supplementation for COVID-19 India
- NCT04476680 Reducing Asymptomatic Infection With Vitamin D in Coronavirus Disease UK
- NCT04476745 The Effect of D3 on Selected Cytokines Involved in Cytokine Storm in the Covid-19 Uninfected Jordanian People Jordan
- NCT04482673 Vitamin D Supplementation in the Prevention and Mitigation of COVID-19 Infection USA
- NCT04483635 PRevention of COVID-19 With Oral Vitamin D Supplemental Therapy in Essential healthCare Teams Canada
- NCT04487951 N-terminal Pro B-type Natriuretic Peptide and Vitamin D Levels as Prognostic Markers in COVID-19 Pneumonia Egypt
- NCT04519034 Vitamin D Status and Immune-inflammatory Status in Different UK Populations With COVID-19 Infection UK
- NCT04525820 High Dose Vitamin-D Substitution in Patients With COVID-19: a Randomized Controlled, Multi Center Study Switzerland
- NCT04535791 Efficacy of Vitamin D Supplementation to Prevent the Risk of Acquiring COVID-19 in Healthcare Workers Mexico
- NCT04536298 Vitamin D and COVID-19 Trial USA
- NCT04552951 Effect of Vitamin D on Morbidity and Mortality of the COVID-19 Spain
- NCT04579640 Trial of Vitamin D to Reduce Risk and Severity of COVID-19 and Other Acute Respiratory Infections UK
- NCT04621058 Efficacy of Vitamin D Treatment in Mortality Reduction Due to COVID-19. Spain
- NCT04628000 Baseline Vitamin D Deficiency and COVID-19 Disease Severity USA
- NCT04636086 Effect of Vitamin D on Hospitalized Adults With COVID-19 Infection Belgium
- NCT04709744 Impact of Vitamin D Level and Supplement on SLE Patients During COVID-19 Pandemic Egypt
- NCT04733625 The Effect of Vitamin D Therapy on Morbidity and Mortality in Patients With SARS-CoV 2 Infection Egypt
- NCT04738760 Clinical Outcomes of High Dose Vitamin D Versus Standard Dose in COVID-19 Egyptian Patients Egypt
- NCT04793243 Vitamin D3 Levels in COVID-19 Outpatients From Western Mexico Mexico
Evidence from treatment trials
Clearly, observational studies are prone to bias, and interventional research is needed to understand clinical effects of vitamins and micronutrients - including the effect size and potential side effects. Among the different vitamins and micronutrients discussed, vitamin D and vitamin C had been studied most extensively regarding their role in the management of respiratory tract infections in the years before COVID-19 and generated the strongest evidence regarding efficacy and safety. A Cochrane meta-analysis focusing on the role of oral vitamin C for the prevention and treatment of common colds, which was updated in 2020 with a total of 30 randomised and nonrandomised trials, reported no consistent effect of daily supplementation with vitamin C in large doses to prevent colds, but modest benefits in reducing duration of cold symptoms [24]. The effect was more consistent in subjects on continuous supplementation and in those performing strenuous exercise. For vitamin D, a very recent updated systematic review and metaanalysis of individual participant data in 2021 investigated the effects of supplementation to prevent acute respiratory tract infections based on 43 eligible randomised controlled trials and a total of 48,488 participants [25]. According to the analysis, vitamin D supplementation reduced the relative risk of acute respiratory tract infection by about 8% (61.3% vs 62.3%) with the strongest effects in patients receiving daily or weekly boluses. There is also interventional research showing that a nutritional support strategy including micronutrients among other reduces adverse outcomes and mortality among malnourished patients [26], but it remains unclear whether micronutrients or support with protein and calories was the main driver of effects.
Most importantly, a number of randomised controlled trials have recently investigated effects of vitamin C and vitamin D supplementation and/or treatment on the risk for COVID-19 infection, as well as treatment courses of infected patients (table 1, lower part). These trials, however, ranging from 54 to 240 patients, did not report significant benefits except for one very small Spanish pilot study [22]. This parallel pilot randomised open-label, double-masked clinical trial found significant differences in the risk for intensive care unit (ICU) admission of patients receiving vitamin D vs not receiving vitamin D (50% vs 2%). None of these trials selected patients with deficient vitamin D levels before beginning the supplementation, the group of patients most likely to benefit from treatment.
Clearly, there are today insufficient data from randomised trials regarding the clinical benefits of vitamin and micronutrient supplementation overall, and more specifically regarding COVID-19. Importantly, however, when looking at the trial registration database (https://clinicaltrials.gov/), there is a high number of registered trials currently planned or ongoing (table 2), which will likely improve our understanding of the role of vitamins and micronutrients in the near future and provide more definite evidence regarding clinical benefits.
Conclusions and implications for patient care
Before answering the question regarding usefulness of supplementation of the population during a pandemic with vitamins and micronutrients as a public health strategy to reduce COVID-19 associated morbidity, it is important to define the level of evidence that is needed. Although there is evidence from preclinical and observational studies linking different vitamins and micronutrients to a well-functioning immune system, interventional research has been rather disappointing and/or lacking. A major problem is the fact that previous trials did not select patients according to the degree of deficiency, and a beneficial effect of supplementation in a person with normal or high levels cannot necessarily be expected. One could argue that it is reasonable to select an entire group of subjects at risk for acquiring severe COVID-19 for supplementation without knowing their level of deficiency, even if only those with deficiency would benefit - particularly if supplementation does not cause harm and is at low treatment cost. Many physicians would follow such a pragmatic view, whereas others prefer a more puristical attitude and would like to wait for more solid trial-based evidence. This dilemma cannot be resolved at the present time. It is not uncommon for public health measures that recommendations are based mainly on observational studies instead of randomised controlled trials, as such trials are challenging, expensive and time consuming. Examples are the recommended reduction of dietary salt or of added sugar.
Such a strategy makes sense if
- most of the experimental and observational evidence points toward a beneficial effect,
- show little or no risk,
- low cost, and
- randomised intervention trials are not feasible in free-living populations.
Such a strategy may also be appropriate during times of a pandemic where time is most precious.
The strongest evidence today is available for vitamin D, with large and high quality trials and meta-analyses from such trials proving effectiveness for prevention of respiratory infections, particularly in patients with deficient levels, receiving daily or weekly boluses. Whether these effects remain true for COVID-19 is currently uncertain. There is no evidence for harm when using vitamin D in doses up to 2000 units per day. For larger doses, however, an increase in falls and other adverse outcomes is possible. Importantly, a significant proportion of elderly patients in Switzerland and other countries do have deficient levels. And this group of subjects is also the one with the highest risk for a severe course of COVID-19.
One (theoretical) concern with improving immune function through supplementation of vitamins and micronutrients is a possible overstimulation of the inflammatory response, which has been shown to be a main driver for COVID-associated pneumonitis and associated mortality and morbidity. There is today, however, no data suggesting that micronutrients and vitamins would do any harm in COVID-19. Importantly, there are many trials currently planned and ongoing, which will increase our current understanding of the role of vitamins and micronutrients for prevention and treatment of COVID-19. Pending results of such trials, it would seem premature to strongly recommend multiple supplementations of high doses of different micronutrients and vitamins to the overall population. For vitamin D, however, the currently recommended supplementation of 800 units per day for the vulnerable population should be underscored, based on possible beneficial effect on COVID-19, besides its proven effects on bone and muscle. Such a recommendation has clearly more upsides than downsides and may alleviate the heavy burden of this devastating disease [27]. In addition, it is time to conduct high-quality trials to better understand whether and which supplementation for which group of subjects is indeed effective in improving immune defence and thereby lowering the burden of COVID-19. Specifically, this includes observational studies looking at the level of different vitamins and micronutrients in different populations to better understand at-risk groups, as well as interventional research to understand which vitamins and micronutrients (in what doses) provide most benefits. Only time will tell whether early implementation of such a public health strategy, as promoted by Berger and colleagues [6], will in the end save lives, and to what costs.
VitaminDWiki
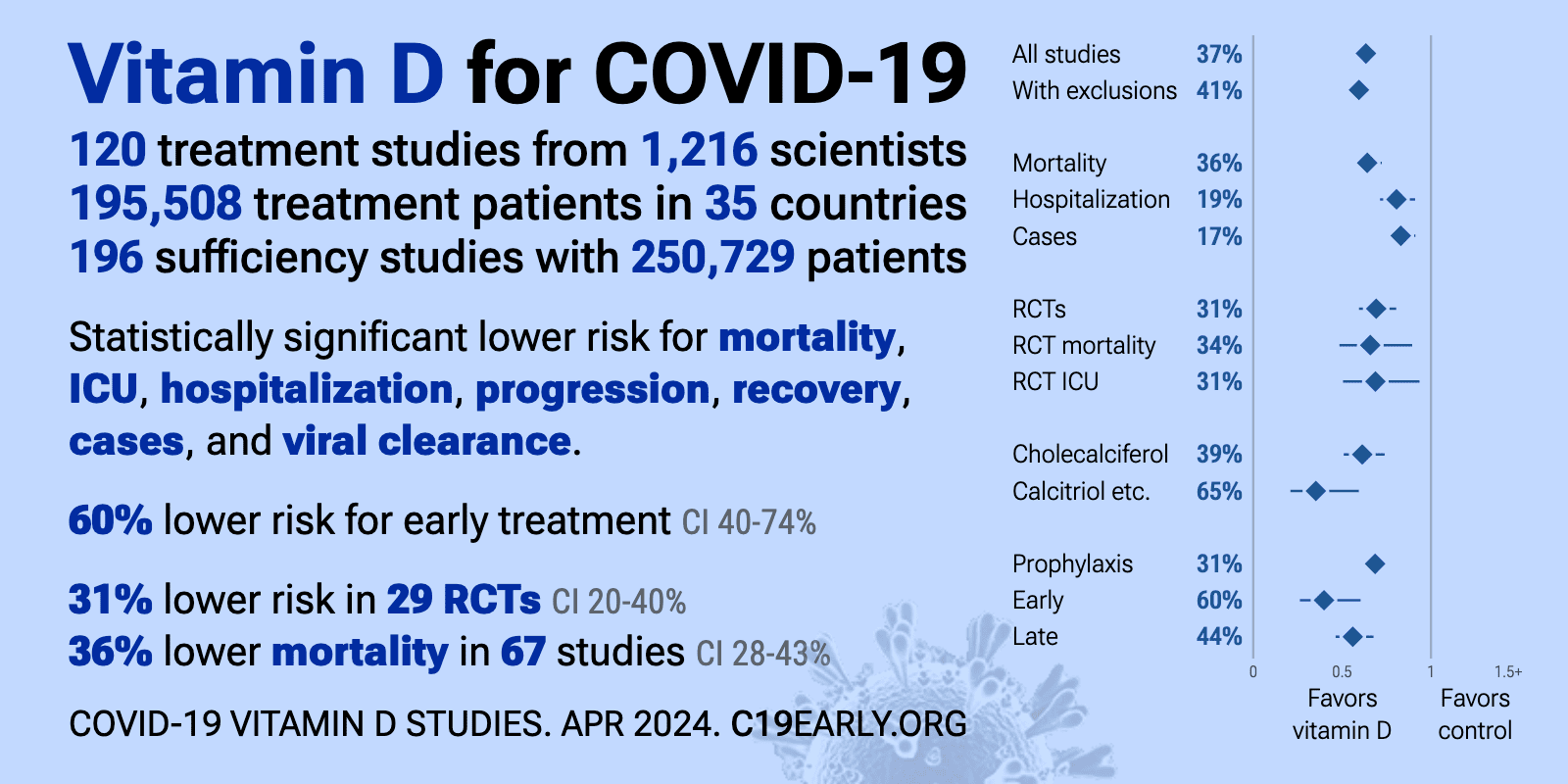
Vitamin D meta-analyses for COVID-19 (auto-updated)
- COVID ICU use reduced by 42% if take more than 100,000 IU of vitamin D over two weeks – meta-analysis Sept 2024
- Vaccinations did not stop COVID (68 studies) – meta-analysis May 2023
- Influenza risk cut in half by the only trial giving enough vitamin D for body weight – meta-analysis Jan 2022
- Multiple Vitamin D doses reduced COVID ICU by 2.5 X , Mech. Ventilation by 5.5 X – meta-analysis May 2024
- COVID death rate in hospital halved if take any amount of vitamin D for any length of time – meta-analysis May 2024
- COVID and Vitamin D: 2X more likely to die if low, 2X more likely to survive if supplement – umbrella meta-analysis April 2024
- COVID fought by Vitamin D: 2.3X less likely to die of COVID if supplemented, 1.9 X less likely to become infected – meta-analysis March 2024
- COVID Vaccinations increased risk of cardiac deaths in youths by 19% - Aug 2023
- T1 Diabetes increased by 27% by second year of COVID – meta-analysis June 2023
- Yet another reason to take Vitamin D while pregnant – fight COVID - meta-analysis May 2023
- COVID death 1.5 X less likely if high vitamin D, emergency D (50K to 100K) is great – meta-analysis March 2023
- COVID ICU 3X less-likely if take any amount and type of Vitamin D – meta-analysis Jan 2023
- COVID and Vitamin D: any amount of D, at any time, for any duration reduced ICU - meta-analysis Dec 2022
- Worse COVID during 3Q pregnancy if 2.5 ng lower Vitamin D – meta-analysis Sept 2022
- Severe COVID 2.6 X less likely if supplement with Vitamin D – 26th meta-analysis - July 2022
- COVID Long-Haul prevalence increases with time: 50% at 4 months - meta June 2022
- COVID test positive is about half as likely if have Vitamin D – 24th meta-analysis - Jan 2022
- Small amounts of Vitamin D reduce Influenza risk by 22 percent (loading dose is far better) – meta-analysis Jan 2022
- Vitamin D fights COVID (54 studies of 1,400,000 people) – 23rd meta-analysis - Dec 2021
- COVID-19 treated by Vitamin D (reduce ICU by 3X) - 22nd meta-analysis - Dec 29, 2021
- COVID-19 death increased 2X if low Vitamin D (less than 10 to less than 30 ng) – 21st meta-analysis Dec 2021
- COVID-19 risk reduced by vitamin D supplementation – umbrella review of 7 meta-analysis – Oct 2021
- COVID-19 treated by Vitamin D (example: ICU reduced by 5X) – 20th meta-analysis Oct 13, 2021
- Severe COVID-19 2.5 X more likely if low vitamin D (23 studies) – 19th meta-analysis Oct 2021
- COVID-19 mortality extrapolates to zero at 50 ng of vitamin D – 18th Meta-analysis Sept 2021
- COVID-19 death 1.6 X more likely if low vitamin D (24 studies) – 17th meta-analysis Aug 2021
- Severe COVID-19 5X more likely if low vitamin D (23 studies) – 16th meta-analysis July 2021
- Severe COVID-19 3.5 more likely if low vitamin D (30 studies) – meta-analysis July 2021
- COVID-19 patients who had supplemented with Vitamin D were 3X less likely to enter ICU – June 2021
- Low Calcium associated with severe COVID-19 – several studies
- COVID-19 mortality 3X more likely if low vitamin D (999,179 people) – meta-analysis March 29, 2021
- COVID-19 was 2.6X more severe if very low Vitamin D (43 studies) – meta-analysis March 26, 2021
- Low Vitamin D associated with 2.7X more severe COVID-19 – 12th MA March 5, 2021
- Vitamin D supplementation fights COVID-19 – 11th meta-analysis Jan 24, 2021
- 3.7 X less likely to die of COVID-19 if supplemented with Vitamin D - meta-analysis Jan 5, 2021
- Less likely to test positive for COVID-19 if higher Vitamin D – meta-analysis Jan 6, 2021
- Vitamin D reduces COVID-19 by 80 percent - anonymous meta-analysis - Jan 5, 2021
- COVID-19 1.7X more likely to be severe if low Vitamin D - meta-analysis Oct 2020
- Low Vitamin D associated 1.8X increased risk of COVID-19 death in hospital – meta-analysis Nov 4, 2020
- Acute viral respiratory infections (RTI) reduced by Vitamin D - 20 reviews - Aug 2020
- Prudent to consider that Vitamin D has a role in COVID-19 – meta-analysis – Aug 7, 2020
- Risk of enveloped virus infection is increased 50 percent if poor Vitamin D Receptor - meta-analysis Dec 2018
- Hepatitis B patients have 2 ng lower level of Vitamin D – meta-analysis June 2019
- Influenza Vaccination not benefited by lowish levels of vitamin D – meta-analysis March 2018
COVID-19 data (auto-updated)
COVID-19 treated by Vitamin D - studies, reports, videos
- As of March 31, 2024, the VitaminDWiki COVID page had: trial results, meta-analyses and reviews, Mortality studies see related: Governments, HealthProblems, Hospitals, Dark Skins, All 26 COVID risk factors are associated with low Vit D, Fight COVID-19 with 50K Vit D weekly Vaccines Take lots of Vitamin D at first signs of COVID 166 COVID Clinical Trials using Vitamin D (Aug 2023) Prevent a COVID death: 9 dollars of Vitamin D or 900,000 dollars of vaccine - Aug 2023
5 most-recently changed Virus entries
All 26 health factors which increase the risk of COVID-19 are associated with low vitamin D
__From CDC
- - - - - - - - - - - - - - - - -
| Sometimes | A health problem will cause a Vitamin D deficiency |
| Sometimes | A Vitamin D deficiency will cause another health problem |
| Always | Stop a vitamin D deficiency to avoid getting additional health problems |
Clinical trials for Vitamin D and COVID-19